Common questions about EOBs
Who can get an Explanation of Benefits?
All members receive an Explanation of Benefits per claim.
Any member who is automatically enrolled or opts in to paperless EOBs can access them through their LifeWise account. If members opt out of paperless and choose to receive printed EOBs by mail, they will still receive an EOB for each claim.
Members have the right to request a paper EOB anytime free of charge. There is no charge to receive either paper or paperless EOBs.
Why is an EOB important?
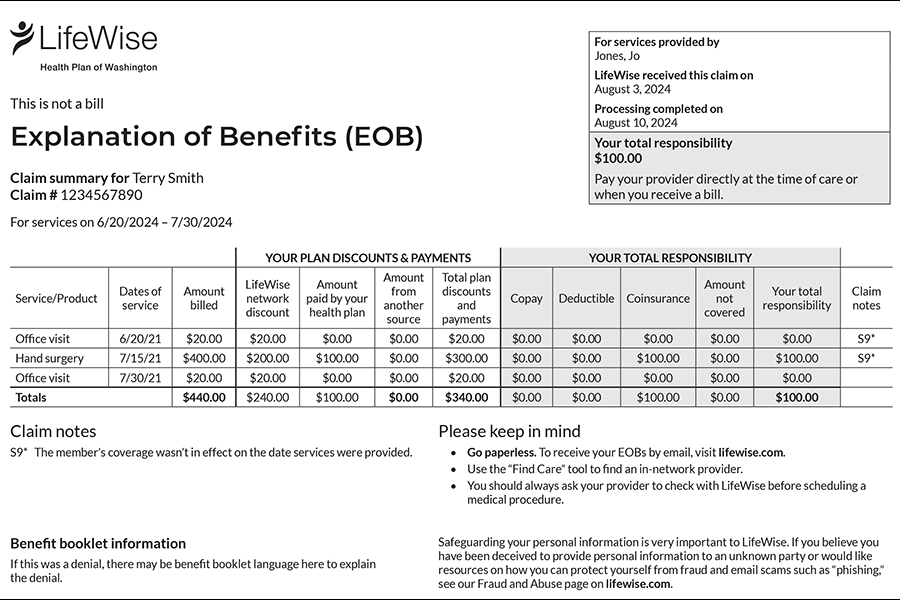
Explanation of Benefits (EOBs) are documents that help you understand your healthcare costs and responsibilities. They outline how and when a claim is paid and who pays for what part of the cost. Your health plan benefits and coverage are outlined in the EOBs.
The EOB is not a bill. It simply explains how your plan benefits apply to that claim. It includes:
- Date you received the service
- Amount billed
- Amount covered
- Amount LifeWise paid
- Any balance you’re responsible for
- How much has been credited toward your deductible
You will receive a separate bill from your healthcare provider for any payment owed. We recommend comparing that bill to your EOB, and then paying the provider directly.
Who can get paperless EOBs?
Who can sign up? Anyone included on your plan who has created their own account on LifeWise.com.
- Plan subscribers
- Other adults on that plan
- Dependents at least 13 years old
Who can't sign up?
- Dependents 12 and under. Their EOBs can be viewed by the plan subscriber.
- Members whose coverage has ended. They receive any further EOBs by mail.
How do I sign up for paperless EOBs?
For individual plans bought via Washington Health Plan Finder:
Go to welcome, then settings in your web account to choose paperless preference.
For employer-based Clark County plans:
Go to Account Settings in your web account to choose paperless Explanation of Benefits.
How do I access my EOBs?
Your Explanation of Benefits are attached to each claim in the web portal.
Find Explanation of Benefits attached to each claim when they are ready to view.
You will be notified by email when new EOBs are ready to view. To update your email address, account settings.
How long before an EOB is created?
An Explanation of Benefits (EOB) is generated as part of your claim being processed. While times may vary, usually EOBs are processed within a couple of weeks of a claim received from a provider or member.
Why does the EOB I received in the mail not match the digital copy?
Why does the EOB I received in the mail not match the digital copy?
An Explanation of Benefits (EOBs) reflects the known cost and coverage details at a certain time. There may be more information between a provider and LifeWise that is processed after the initial claim was submitted. An EOB received later may reflect updated cost and coverage details.
Why don't I have EOBs for pharmacy claims?
EOBs are not provided for pharmacy claims, but you can find how drugs and your pharmacy benefits are covered via your benefit booklets or other pharmacy benefit materials.